This story appeared in the spring 2014 issue of Chapman Magazine.

It was a mouthful of a diagnosis: De Quervain’s tenosynovitis, a painful condition that made the bottom of her thumb and the side of her wrist hurt. But Nancy thought of it more simply. It was knitter’s thumb, kind of like tennis elbow without the athleticism. She had been on a tight deadline to finish her grandchild’s baby blanket before the estimated due date, two weeks hence. She spent long, uninterrupted evening hours knitting one, purling two — over and over. Then the pain hit. Not only could she no longer knit; she could barely hold a fork to eat.
She called her doctor’s office, in this hypothetical picture of the new world of health care, but her primary physician was booked solid. She got right in to see his physician assistant. She went home with a splint for her thumb and wrist, advice to avoid using the hand, and recommendations for ice and ibuprofen for pain relief. Behind the scenes was a consult between the P.A. and a physical therapist that confirmed the diagnosis, recommended the splint and scheduled an appointment for follow- up therapy. Nancy never saw her primary care physician for the pain. But at her next physical exam, he glanced at her record and said, “So, how’s the thumb?”
In the not-so-distant past, Nancy might have felt she had no choice but to wait for an appointment with her doctor. Or the pain might have driven her to an emergency room, the most costly setting for healthcare services. In the U.S., the average cost of an emergency room visit for a sprain or strain is $1,051.
In today’s evolving healthcare environment, a team approach is increasingly likely. Chapman University students are on the cutting edge of training for that new healthcare paradigm.
Hopes are that team medical care will begin to address a costly and often dangerous void
in America’s healthcare system that has long rewarded more, not better, care. In that system, no one doctor is paid to communicate with other medical providers. No one is paid to scrutinize new prescriptions and make sure they don’t interact with medications patients already take. Caregivers are not paid to communicate with each other, even as patients are referred from one health expert to another.
Models for change take on various names, including ACOs and patient-centered medical homes. But the team approach is central, regardless of the name. A physician leads each network, but teams could well have a variety of members, depending on the patient’s needs. The team might include a physician assistant, a nurse practitioner, a pharmacist, a nutritionist, a physical therapist, a mental- or behavioral-health specialist, or any number of highly trained experts to helpthe patient. All keep the patient’s needs paramount as each team memberworks to the maximum scope of his or her training.
It’s shaping up as a huge national experiment, giving providers a financial incentive to work together; promising to save money by avoiding duplicative tests, unnecessary procedures and dangerous drug interactions; and making the team jointly accountable for the health of patients. None of it will work unless each member of the team seamlessly shares information with the others.
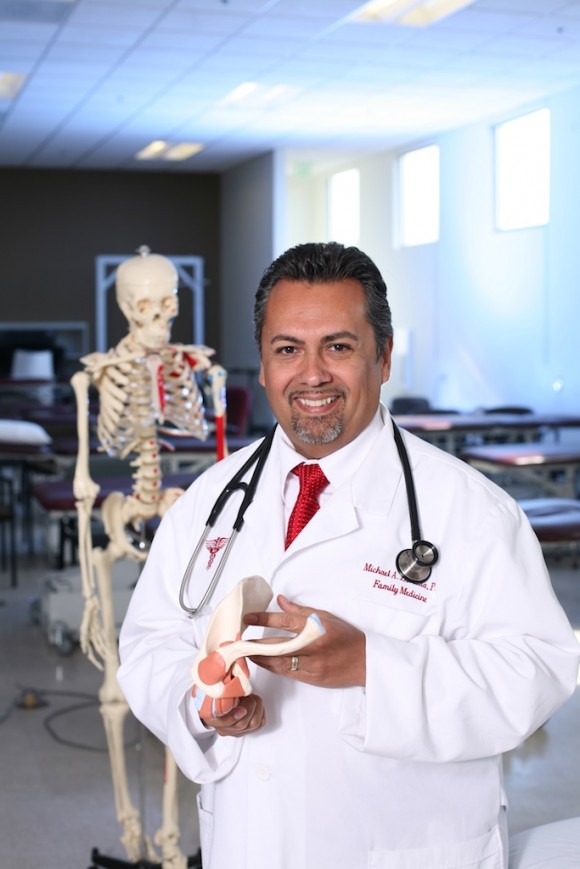
Chapman has launched two new health-science programs that will add well-trained providers ready to answer the call for team medical care. Michael Estrada, founding director of the Physician Assistant Studies Program in the Schmid College of Science and Technology, expects to welcome new students in 2015. And Ron Jordan, R.Ph., FAPh.A, is the founding dean of the new Chapman University School of Pharmacy (CUSP), which plans to welcome students to the professional portion of its program in 2015. Existing University programs, including physical therapy and communication, are on board with their own emphasis on the team approach to medicine.
Primary-care physicians are going to need all the professional help they can get. The next few years will see an influx of millions of newly insured Americans, all looking for a primary-care provider. Predictions are that by 2025, the United States will suffer a shortage of up to 45,000 primary-care providers.

Physician assistants are already geared up for practicing medicine as part of a team, and they, along with nurse practitioners, will be just what the country needs to
help ease the physician shortage.
“Physician assistants provide a broad range of medical services, from assisting primary-care providers to assisting in surgery and prescribing medication,” says Estrada. “They work as a team with a supervising physician, but within that relationship they make autonomous decisions.” The P.A. works in partnership with a physician, but not necessarily side by side. Their relationship can be in the same room, over the phone or via email and other electronic communications.
The P.A. Nancy saw for her “knitter’s thumb” could act independently. State laws vary, but in California a physician is required to review 5 percent of the medical records initiated by a P.A., though the physician eventually will have access to details of all P.A. encounters next time he or she sees the patient.
That expertise and flexibility allow P.A.s to fill in provider gaps in rural
or urban areas that have long been underserved. They might have careers
in a family practice office, a specialty office, a long-term or acute care facility
or dozens of other healthcare settings. According to the American Academy of Physician Assistants, P.A.s are prepared to perform 85 percent of the duties performed by a physician. “The Affordable Care Act is pushing this forward. We’re poised and ready,” says Estrada.
Orange County has one of the largest homeless populations in Southern California. That’s one reason that the Chapman P.A. program will train its students not only
in medical science, but also in the mental and behavioral sciences. And the program will give students experience in cultural diversity, seeking training partnerships
with community healthcare clinics that provide services to immigrant populations and poor and homeless people.
“We’ll see working folks, including those who have lost their jobs, maybe even their homes,” says Estrada. “They still need physical exams. Their school-aged kids still need immunizations. They’ll have a medical home, so they won’t find themselves in
an emergency room for routine care.”
There will be a host of others on the team, and P.A.s will draw on diverse health- care expertise. If someone is depressed, a P.A. could refer to the team’s mental health therapist. If obesity is a central problem, a nutritionist, dietician or exercise therapistmight best serve the patient. Following stroke, an accident or an overuse injury — like Nancy’s knitter’s thumb — a physical therapist enters the patient’s care circle.
Or a pharmacist will get involved. “If a patient is on multiple medications, the best person to manage that will be a pharmacist,” Estrada says.
Pharmacists will take a more hands-on approach with patients. Nearly half the population in the United States took at least one prescription drug in the past month, according to a 2008 survey by the Centers for Disease Control and Prevention; among those aged 60 and older, more than three-quarters used two or more prescription drugs, and 37 percent of those elderly patients used five or more. Each additional drug increases risks of harmful drug interactions.
“For 15 years, I was an assistant area medical director at Kaiser Permanente in Orange County,” says Dr. Richard Pitts ’70, D.O., Ph.D., chief medical officer and interim CEO of Arrowhead Regional Medical Center in Colton, Calif. “That environment is all about teams. If you have a blood clot and use a blood-thinning agent, that management is done by pharmacology, not by a physician.”
Drug therapy, which may one day include individual genetic profiles, is sure to become more complex. “Pharmacists are the medication therapy experts,” says Jordan. “They
receive more hours of training on the use and science behind medications than any other healthcare practitioner.”
The pharmacist of the future will be a people person, accessible without an appointment, and Chapman is looking for students who can help lead the kind of cultural change that pharmacies of the future will require. No longer the unseen experts in the recesses of the drug store, pharmacists will be familiar faces to patients looking for advice.
“We’re looking for the (student) who will have a strong relationship with patients,” says Siu Fun Wong, PharmD, FASHP, FCSHP, associate dean of assessment and scholarship and professor of oncology at the Chapman University School of Pharmacy. “They’ll need to have knowledge, skill and confidence in their abilities. Add to that an attitude of wanting to work with people.”
The Accountable Care Organization provision in the Affordable Care Act encourages doctors, hospitals and other healthcare providers to form networks to better coordinate care. Already, some 4 million Medicare beneficiaries are in ACOs, and 428 hospitals have signed on to the concept. Overall, about 14 percent of Americans are in an ACO. Millions more find themselves being cared for by patient- centered medical teams accountable for meeting the majority of patient needs, including prevention, wellness, acute care and chronic care.
One such model, Belmar Family Medicine in Lakewood, Colo., has been recognized since 2009 as a fully qualified patient-centered medical home by the National Center for Quality Assurance. The core team consists of two physicians, Dr. Tracy Hofeditz and Dr. Kristin Marie Everett, and a nurse practitioner. A care coordinator backs them up. She monitors patients to ensure control of such things as blood pressure, arranges referrals to specialists, orders laboratory work and makes sure transitions of care and medical documentation are complete. Two medical assistants greet and check in patients at the practice. They take vitals, measure weight and height, ask about all medications patients are taking, update medical records and provide a written plan as well as a verbal review of instructions after each visit. A part-time mental-health expert sees patients who test positive on depression screening, and a pharmacist is consulted for complicated medication questions.
In the old way of practicing, doctors may have felt overwhelmed by the introduction of a new screening test, such as for depression. Now, says Judy Hewitt, Belmar’s practice manager, the mental- health expert takes that burden from their shoulders and follows up with expert care for depressed patients right in the practice’s offices. That kind of immediate support frees doctors to spend precious time with patients — the elderly or those with multiple chronic problems — who have complicated needs.
“Becoming a patient-centered medical home has changed the role of a provider to one of being a change agent,” says Hewitt. “It may mean the patient goes to a mental health therapist, or a weight loss program, or takes medications differently. It’s a team effort. Everyone is working toward helping the patient get better and stay better.”
For some healthcare experts, a team approach is old news.
“Physical therapists have been members of the healthcare team since the inception of the profession,” says Alison McKenzie, Ph.D., professor in Chapman’s Department of Physical Therapy. P.T.s educate patients and show them how poor movement and health habits can contribute to their problems.
With everyone in sync, the team-care net expands. Traditionally, physical therapists have reached out, adding patients’ loved ones to the team.
“We involve family members and caregivers, educating them about the role of behavior and choice in the health and wellness of the patient,” says Jacklyn Brechter, Ph.D., chair of the Department of Physical Therapy.

So we can assume, for the knitter’s thumb example, that the P.T. would have been delighted
to welcome Nancy’s husband as the newest member of her care team when he accompanied her to the appointment. As he watched and listened, he could prepare himself to cajole his wife to do recommended exercises, and to limit the time she spent knitting.
Team care can only succeed if each member in a patient’s care talks to the others involved.
“Communication by healthcare providers has been linked to patient satisfaction and compliance,” says Lisa Sparks, Ph.D., Foster and Mary McGaw Endowed Professor in Behavioral Sciences and director of the Health and Strategic Communication Program at Chapman.
In every aspect of team medical care, the ultimate focus is the patient. “Team members change, but the client is always there, at the center,” says Judy Montgomery, Ph.D., program director, Communication Sciences and Disorders in the College of Educational Studies at Chapman.
Says Hewitt, who has been with the Lakewood, Colo., practice through its transition from a traditional-care to a patient-centered medical homecmodel: “We’d never go back to the way it used to be.”





Add comment