Janet Johnson was in her Los Angeles home when her smile became crooked and her voice slurred. A few hours later, she was lying in a hospital bed, and half of her body was paralyzed.
In an instant in 2009, a stroke changed the trajectory of Johnson’s life and she faced years of recovery to rebuild the bodily autonomy that she lost.
That battle became all the more difficult when she was asked to leave a rehabilitation facility because her insurance wouldn’t cover more than three months of physical therapy.
“I was completely devastated,” Johnson said. “What I heard was, I have to stay like this for the rest of my life.”
But that wasn’t an option for Johnson, who had been taking care of her sister since she suffered a traumatic brain injury in a car accident. Fortunately, Johnson connected with a program at Chapman University that helps rehabilitate stroke victims through novel technology and personalized care at no cost to patients.
Johnson and her sister have been attending the stroke boot camp once or twice a year ever since.
“It’s been a lifesaver for both of us,” Johnson said. “I am able to take care of myself and my sister. That’s what matters.”
Johnson’s story shows just one of the many ways that Chapman University is answering the needs of an aging population locally and nationally. Investment in graduate health programs is one of the pillars of the university’s five-year strategic plan.
Within the university’s Crean College of Health and Behavioral Sciences and School of Pharmacy, faculty and students are producing groundbreaking research, contributing to impactful community programs and designing curriculum to improve quality of life for the aging population of Orange County and beyond. They are the architects of new health-care models that could help solve a looming emergency.

Addressing Health Care for Older Adults
While the entire country is facing a shift in demographics, Orange County — the sixth most populous county in the United States — serves as a perfect representative sample. Nearly one in four residents in Orange County will be 60 or older by 2040 compared to 14.3% in 2019, according to the Orange County Health Care Agency. This presents several challenges, mainly because there aren’t enough health-care providers in the county to care for these older adults, and many are not well-versed in caring for an older population.
Crean College Dean Janeen Hill said the county will need about 40% more physician assistants, speech language therapists and physical therapists, respectively.
“The world is getting older, but if you want a case in point of where we are in this crisis, it’s Orange County,” Hill said. “We just need a whole lot more health-care providers who are trained in these specific areas.”

Pronounced racial and socioeconomic health disparities in the county could also play a role in limiting the ability of older adults to access specialized care. If an older adult belongs to an underrepresented group, they may lack access to necessary health care in Orange County and the rest of the country, Hill said.
“The expense of health care is another major problem,” Hill said. “Not everybody can afford specialty care and so we know there’s enormous disparities.”
With these obstacles in mind, Hill and other Chapman health leaders have put together programs and partnerships from which older community members already benefit. The influence of the university is also being felt in the vital research that will lead to new treatments and the students who go out into the world with a profound sense of purpose and unique skill sets from working with older adults.
“Since Chapman President Daniele C. Struppa came to Chapman as provost in 2006, he has been very clear that a university needs to be relevant to the community,” Hill said. “A university cannot be an ivory tower, isolated from what’s important to the community. We need to be offering programs that are relevant. We want the relationships with our community to be built around the fact that Chapman will solve problems that impact them, and this is a big one.”
Training Tomorrow’s Health Leaders
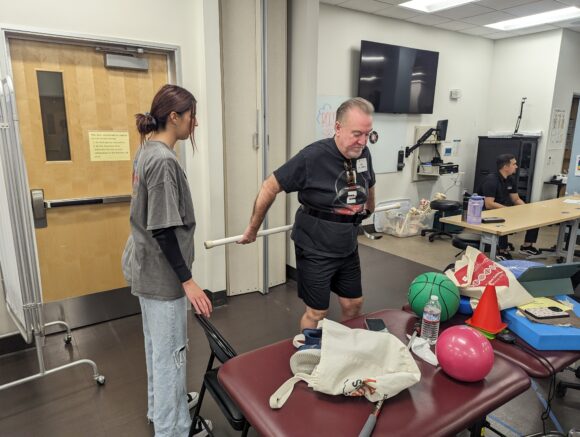
Crean College has several community programs that benefit local patients and students. One of these initiatives is the bi-annual stroke recovery boot camp that has improved the lives of many community members like Johnson and her sister. Students are gaining invaluable hands-on experience while helping patients re-learn motor skills and other daily living abilities.
The program serves a dual purpose—supporting members of the community who may not be able to afford specialty care and training the next generation of medical practitioners who will care for older adults with a greater understanding of personalized health care.
“We know it’s imperative that as we grow our graduate health professional programs, that we do so with an eye toward preparing health professionals to be ready to work with a diverse and aging population,” Hill said. “Through stroke boot camp, our students are being prepared to go out into the community and work with this group of people.”

The program helps empower individuals who have lost much of their autonomy. As Johnson pointed out, many rehabilitation activities are enjoyable for patients. Johnson’s favorite part of the boot camp is playing virtual reality video games to improve various motor skills. She’s also developed friendships that help motivate her recovery.
“There’s something therapeutic about seeing somebody else progress and seeing them over the years,” Johnson said. “I had friends that I used to push in a wheelchair and the next year they’re walking again. It gives you a lot of hope.”
To further support low-income and underserved community members, Crean College has a Simon Scholar Physician Assistant Program that provides free tuition to students from lower socioeconomic backgrounds. In addition to improving these students’ lives, the program also exemplifies Chapman’s commitment to serving all communities in the county. Each student receives a scholarship in exchange for committing to work for three years in a local underserved medical community.
“So we are directly saying to people, we are going to give you the benefit of a wonderful career, and the community will benefit from you going back to serve,” Hill said.
Crean College also has an Adult Learning Lab for other patients with brain diseases, a COVID-19 long hauler clinic and a marriage and family therapy program that teaches caregivers how to look after their loved ones with brain diseases or injuries.
“These programs allow us to put together the kinds of experiences our students need to work in the community, and it is a huge service to people who cannot afford this level of care,” Hill said.
The programs are held at Crean College’s Rinker campus in Irvine, where a new 52,000-square-foot campus center building opened last year in Irvine. The campus is a major part of Chapman’s significant investment in the community’s future. The cutting-edge building serves as a training ground for tomorrow’s health and behavioral sciences leaders and pharmacists who will help administer life-saving treatments to older adults in the community.

Increasing Access to Pharmacists
Age is the greatest risk factor for cancer, cardiovascular disease and neurodegeneration, according to the National Institutes of Health. With older adults taking more medications than ever to treat and prevent these and other diseases, the importance of pharmacists will increase.
Pharmacists are far more accessible than most medical professionals. It can take months to schedule an appointment with a physician or their physician assistant, while pharmacists are regularly available to provide guidance on medications. But alarmingly, there’s already a shortage of pharmacists because young people aren’t generally attracted to the profession. Chapman School of Pharmacy Dean Rennolds Ostrom said this is due to the public’s misconception of what pharmacists do, particularly their role in direct patient care.
“It’s much more than the community pharmacist sitting behind a counter at Walgreens,” Ostrom said. “Physicians don’t know the chemistry or structural elements of medications and how they work. That’s the pharmacist’s job, and physicians rely on them for that.”
Chapman’s School of Pharmacy is uniquely positioned to help care for older adults. Many pharmacy schools nationwide tend to be either large, research-oriented institutions or teaching-focused universities, but Chapman combines strong researchers and personalized teaching programs.
“We have researchers with substantial reputations just like the big universities, but the difference is we have those researchers teaching in the classrooms,” Ostrom said. “By combining excellent, passionate teachers who are also scholars and knowledge creators, we are preparing our students better for the future. Drugs are coming out faster than they have ever in human history, so we have hit that perfect balance in preparing our students.”
To attract more talented students to the profession, the School of Pharmacy offers the Accelerated Pre-Pharmacy Experience Program (APEx), which allows high school graduates to bypass a bachelor’s degree and earn their Doctor of Pharmacy in five years. This means students are becoming practicing pharmacists about three years earlier than it usually takes. This encourages more talented students to enter the field and ensures a quicker pipeline for increasing the number of pharmacists in the community.
The program will also help support older adults in underserved communities. The reduced cost of obtaining a doctoral degree through the APEx program will encourage more underprivileged students to become pharmacists, which could increase the number of pharmacists in communities in need.
“The degree ends up being a lot cheaper because of the time saved,” Ostrom said. “So, we can improve access given the health care deserts that exist particularly in Hispanic communities in our area.”

Research with Purpose
While Chapman is profoundly impacting its local community, the university’s influence is vast. Innovative researchers are producing groundbreaking studies that will help shape how age-related conditions are treated in the U.S.
One of these researchers, Associate Professor Rachita Sumbria, has helped uncover that age contributes to brain hemorrhages. This finding redefines how health-care professionals will view bleeding in the brain, which is associated with stroke and cognitive decline.
Published in the Journal of Neuroinflammation, Sumbria’s study shows that aged red blood cells tend to attach to the tiniest vessels, or capillaries, in the brain. Once these cells attach to capillaries, they are taken into the brain, which can cause microhemorrhages.
The research opens up future possibilities for treatment and prevention, as it was traditionally believed that red blood cells enter the brain through a rupture before causing hemorrhages.
“This can lead to new research and theories that will help us determine how these red blood cells are interacting with the vessels of the brain,” said Sumbria, who is based at Chapman’s School of Pharmacy. “We can then identify molecular targets to begin designing drugs to block those targets. Now that we know that the phenomenon is happening, the next step is to understand what is causing this to occur. Once we get those answers, we can design therapies to block the process.”

The research could also aid further understanding of Alzheimer’s disease, which primarily impacts people who are 65 and older. Sumbria said Alzheimer’s is associated with changes in red blood cells, and patients also have microhemorrhages.
Research into Alzheimer’s is critical as the number of Americans with the disease is projected to grow from 6 million to nearly 13 million by 2050, according to the Alzheimer’s Association. In addition to the physical toll on the patient, the disease also causes profound psychological and financial trauma to families, who often become caretakers for their loved ones diagnosed with Alzheimer’s.
With so much at stake, Chapman faculty are taking an interdisciplinary approach to offering solutions. Professor of Statistics Cyril Rakovski of Schmid College of Science and Technology has been studying large health records data combined with cutting edge analytical techniques to determine the effects of existing treatments on important disease outcomes such as survival probability, frequency of hospital visits, duration of hospital stays and cost of treatment.
With regards to Alzheimer’s, Rakovski and other researchers examined three of the most prescribed drug treatments: Donepezil, Memantine and a combination of both. The compiled data, which was gleaned from two large medical databases, Oracle Health Records Real-Life Data and IQVIA insurance claims data, showed that more than 303,000 people would survive after the fifth year following their initial diagnosis if everybody on a single medication or no medication were switched to the combined treatment. These patients would have died otherwise.
The researchers also found that the combination treatment decreases the amount of hospital visits per year, improving patients’ quality of life. This would lessen the financial impact on patients and their families, reducing annual medical expenses in the U.S. by more than $940 million.
“As the aging population and presence of Alzheimer’s increases, new treatments will become available,” Rakovski said. “But for now, we don’t have to invent anything to improve hundreds of thousands of lives. And if the number of Alzheimer’s patients doubles, the treatment method we highlighted can improve even more lives.”

Changing Lives
As the need for specialized care for older adults rises, the researchers, students and faculty at Chapman will continue to drive positive change in the health-care industry. At both the local and national levels, the university is contributing to enhancing systems of care that are already improving patient outcomes.
Chapman’s work within Orange County is an important example of how universities can pay back communities by solving problems that directly affect the public. This impact is evident in the inspiring stories of recovery of so many community members.
On any given day, Johnson and her sister draw on the lessons they’ve learned and the strength they’ve forged during Chapman’s boot camp to work together to perform the daily functions that once came easily to them. With Johnson losing complete control of the right side of her body and her sister losing the left side, they’ve learned how to support each other, giving strength where each other is weak.
“I found the stroke boot camp at a time when I felt hopeless,” Johnson said. “I didn’t know whether I would be able to take care of myself, let alone my sister. But we learned to work like a synergy. My sister helps me and I help her. Together, we make a complete person, highly motivated and well trained to live successfully. It isn’t perfect, but we’ve learned how to live a happy life.”




