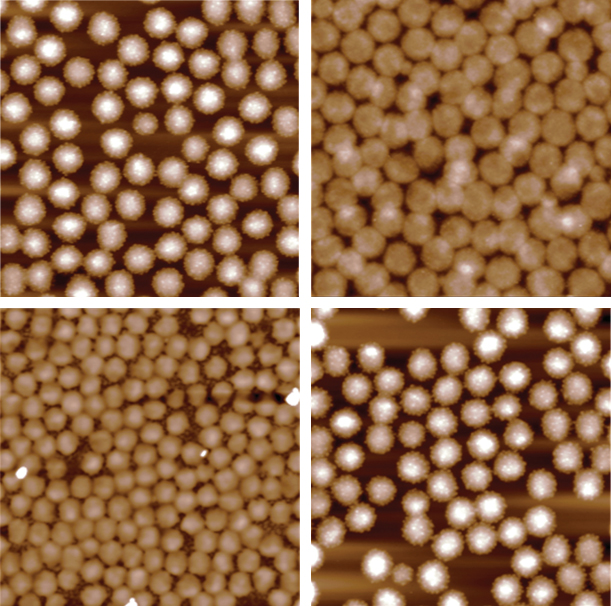
Andrew Lyon’s research world revolves around stretchy bits of science 10,000 times smaller than a human cell. But those nanoparticles hold oversized promise as breakthroughs in the lives of everyone from trauma victims to cancer patients.
The microgels in Lyon’s lab at Chapman University may ultimately be the building blocks for an IV injection that stems uncontrolled bleeding. Or they may get commercialized as a topical powder that first responders pour into a wound to get blood to clot. Then there’s the science fiction scenario: They become a preemptive product that safely flows through the bloodstream of soldiers or others headed into harm’s way so if they sustain a traumatic injury, protection is already in place.
Closest to market is a product that aids patients
whose blood doesn’t clot properly because they’re undergoing chemotherapy.
“If we can use these polymer nanoparticles to commercialize artificial platelets, we can change bleed rates and improve models of survivability,” says Lyon, Ph.D., dean of Chapman’s Schmid College of Science and Technology. “That’s why we’re so excited.”
After nearly 20 years of foundational work in polymer science and soft condensed-matter physics, the science of polymer nanoparticles pretty much flows through Lyon’s own genetic makeup.
“The artificial platelets and how they work is kind of like taking an Isaac Asimov ‘Fantastic Voyage,'” Lyon says.
Using an erasable marker, the dean creates interlocking loops, squiggles and arrows on his office whiteboard as he diagrams the science of his project at the molecular level. The particles at the heart of the research feature a coil-like structure that expands within a fibrin mesh to allow for multiple binding sites, mimicking the architecture of natural platelets.
Lyon uses an analogy: “If you’re putting a stack of papers together, 20 staples are better than one,” the researcher says. “So that’s part of the secret sauce here – a super stretchy polymer that we’ve designed as the body of an artificial platelet that displays thousands of binding sites for natural fibrin.”
Once the platelets bond to a clot, they pull the fibrin polymer in, “almost like a little muscle,” Lyon says. “That makes the clot more stable so the body can step in and regenerate normal tissue.”
These days, Lyon’s team is focusing on scale-up of the project to produce more of the polymer and ensure consistent quality. That will allow for further testing and, ultimately, commercialization.
“Going from a gram of polymer to making 50 grams takes a lot of science and engineering,” he says.
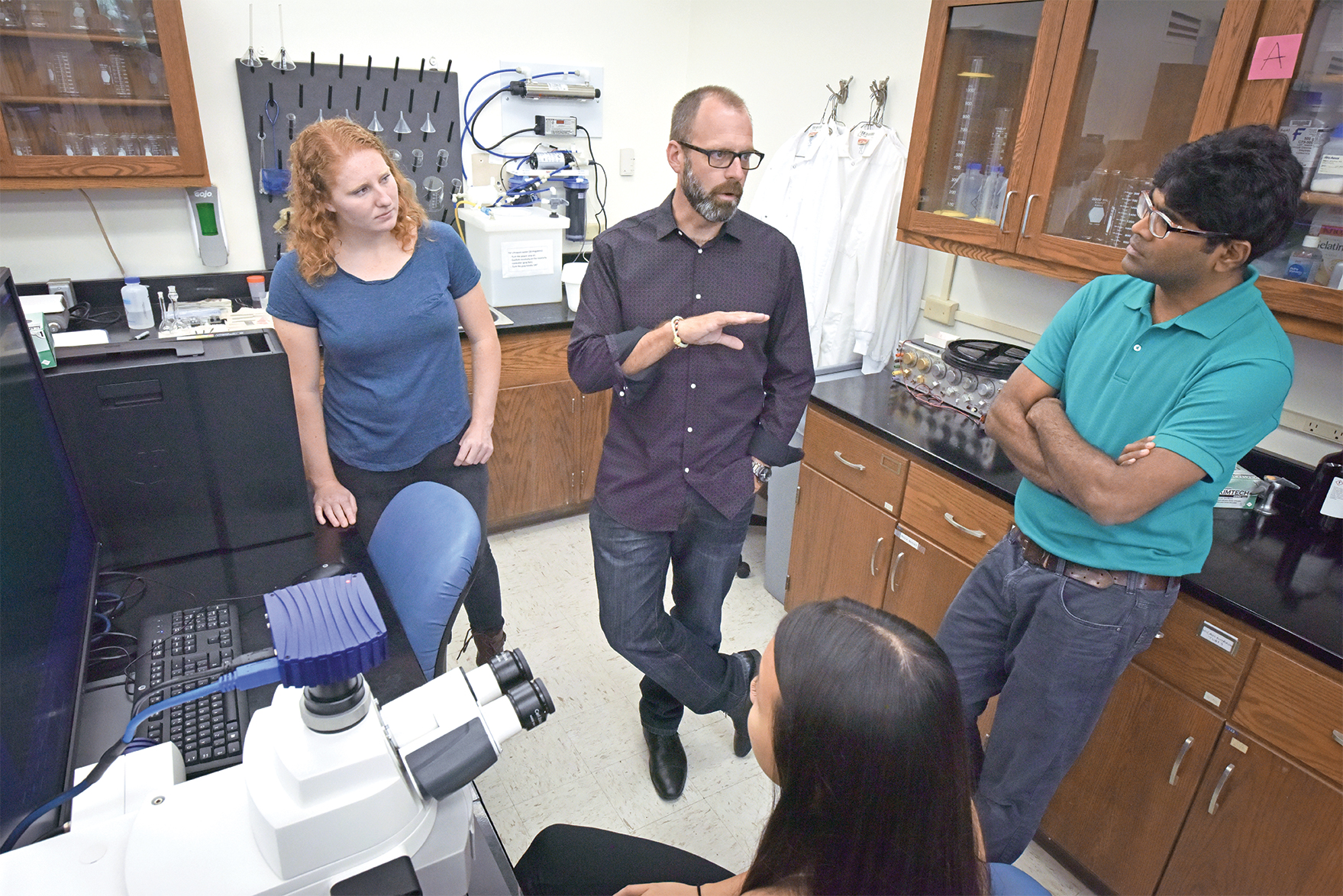
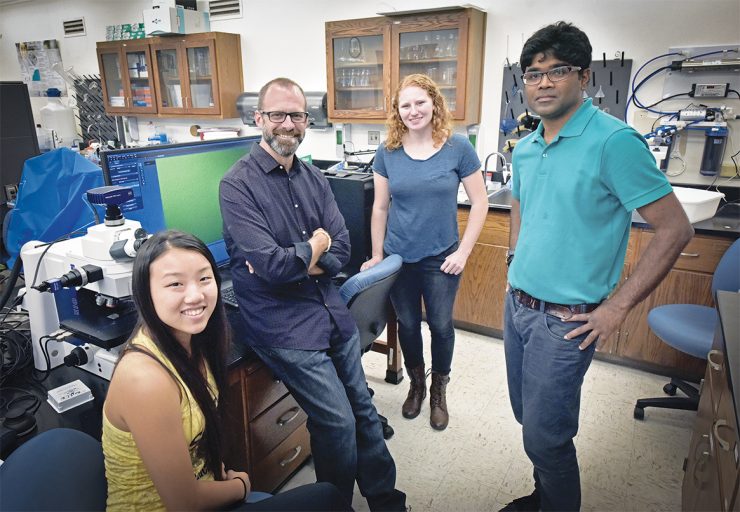
This endeavor is hardly Lyon’s alone. His team at Chapman includes research scientist Molla Islam, Ph.D., as well as Chapman graduate and student researchers. Meanwhile, collaboration crosses campuses and time zones, as Lyon is one of four main investigators on the project. The others are Thomas Barker, Ph.D., a professor of biomedical engineering at the University of Virginia; Ashley Brown, Ph.D., a professor at North Carolina State and UNC-Chapel Hill specializing in regenerative medicine and pharmacoengineering; and Wilbur Lam, Ph.D., of Emory University and the Institute for Electronics and Nanotechnology at Georgia Tech.
It was over a cup of coffee four years ago that Lyon and Barker launched the joint research effort. At the time, they were pursuing a $13 million grant from the Defense Advanced Research Projects Agency (DARPA) for a field-trauma application of their research. Although they didn’t get that grant, the process “made us think deeply about how the technology could be successful,” Lyon says. “So when we got in the lab and started building something, we had a good idea what the design features would be.”
Now Lyon’s team is part of a five-year, multimillion-dollar grant from the National Institutes of Health, and the hope is that the grant will culminate with team members gearing up for a clinical trial.
“All the initial studies are positive,” he says.
As the project advances, transforming from a broad concept discussed over coffee into a biomedical breakthrough, Lyon takes a moment to reflect on the ups and downs along the way.
“I think of science as this constant oscillation between fascination and frustration,” he says. “What you’re really striving for is spending more time on the fascination side than on the frustration side.”
Sure, there are frustrations as team members try to translate research into a reproducible product and then commercialize it. But, oh, the rewards on the fascination side when “you learn something about nature that no one has ever known before,” Lyon says.
“The exciting thing is that we continue to challenge this technology, and now we can see the light at the end of the tunnel,” he adds. “We can see how this will have a positive impact on people’s lives.”
Cover Photo: The polymer research team at Chapman is led by Andrew Lyon, second from left, and includes high school students Vivian Yip, left, and Maddie Tumbarello, as well as research scientist Molla Islam.